Glucagon (1-29) – Human, Porcine (CAS: 16941-32-5)
SB-PEPTIDE offers glucagon 1-29 peptide HSQGTFTSDYSKYLDSRRAQDFVQWLMNT for research on diabetes, obesity, and non-alcoholic fatty liver disease (NAFLD).
G-Protein Coupled Receptor
Glucagon operates through the GPCR signaling pathway, which plays a pivotal role in cellular communication. This type of receptors are known as seven-transmembrane domain receptors, which possess a unique structure that enables them to detect external molecules and activate cellular responses. Their vital association with G proteins fuels a cascade of events, initiating a cellular symphony, orchestrated by two principal signal transduction pathways: the cAMP signal pathway and the phosphatidylinositol signal pathway.
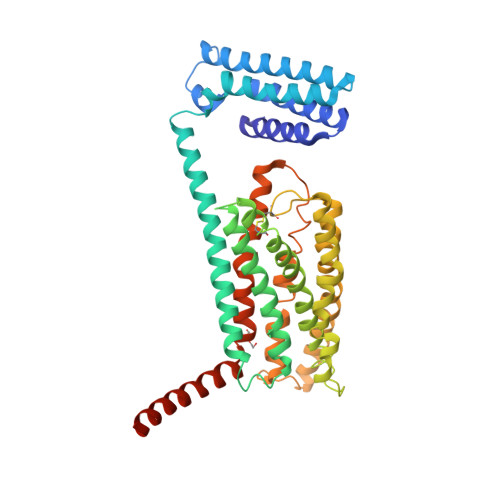
Glucagon class B GPCR 3D structure
Glucagon receptor/class B GPCR
GPCR superfamily is organized into three main classes, among which the secretin receptor family (class B) regulated by glucagon peptides.
Glucagon receptor is a 62 kDa plasma membrane protein activated upon binding to glucagon. When HSQGTFTSDYSKYLDSRRAQDFVQWLMNT binds to its receptor, conformational changes occur, which leads to the activation of G proteins. This activation sets off a cascade of events, including adenylate cyclase activation and subsequent cyclic AMP (cAMP) production. The cellular response is further orchestrated by protein kinase A, initiating series of biochemical reactions.
Thanks to previous studies, it is known that glucagon receptors are predominantly present in the liver and kidneys, with varying expressions in other vital organs. Interestingly, the way glucagon works in diabetes, obesity, and NAFLD has led to new areas of investigation, suggesting its potential use as therapeutic target.
Glucagon(1-29) glucoregulatory peptide hormone
Thanks to its ability to stimulate hepatic glucose production, modulate energy balance, and potentially influence appetite regulation, glucagon 1-29 glucoregulatory peptide (CAS: 16941-32-5) represents a new powerful and versatile tool in driving scientific progress. It’s implication in various realms, ranging from the treatment of severe insulin-induced hypoglycemia to potentially addressing obesity and NAFLD, opens doors to innovative therapeutic avenues.
Let SB-PEPTIDE give you the compass to guide you toward new groundbreaking advancements in medical science. Ask for a quote in one click on this webpage’s upper right button.
For research use only
Technical specifications
 |
Sequence : HSQGTFTSDYSKYLDSRRAQDFVQWLMNT |
 |
MW : 3482,75 g/mol (C153H225N43O49S) |
 |
Purity : > 95% |
 |
Counter-Ion : TFA Salts (see option TFA removal) |
 |
Delivery format : Freeze dried in propylene 2mL microtubes |
 |
Peptide Solubility Guideline |
 |
Bulk peptide quantities available |
Price
| Product catalog | Size | Price € HT | Price $ USD |
| SB178-1MG | 1 mg | 110 | 138 |
| SB178-5MG | 5 mg | 385 | 481 |
| SB178-25MG | 25 mg | 1540 | 1925 |
References
Endocrine-related Cancer. 2023 Jul 28;30(9):e230046. doi: https://doi.org/10.1530/erc-23-0046
One hundred years after the discovery of insulin and glucagon: the history of tumors and hyperplasias that hypersecrete these hormones.
The Journal of Endocrinology. 2023 Jul 01;:JOE-23-0081. doi: https://doi.org/10.1530/joe-23-0081
Metabolic regulation of glucagon secretion.
Journal of Diabetes Investigation. 2023 Apr 13;14(7):829-837. doi: https://doi.org/10.1111/jdi.14009
Newly discovered knowledge pertaining to glucagon and its clinical applications.
Front. Endocrinol. Sec. Diabetes: Molecular Mechanisms. 2022 Jun 16;Volume 13. doi: https://doi.org/10.3389/fendo.2022.928016
Role of Glucagon and Its Receptor in the Pathogenesis of Diabetes
Various theories for the hormonal basis of diabetes have been proposed and debated over the past few decades. Insulin insufficiency was previously regarded as the only hormone deficiency directly leading to metabolic disorders associated with diabetes. Although glucagon and its receptor are ignored in this framework, an increasing number of studies have shown that they play essential roles in the development and progression of diabetes. However, the molecular mechanisms underlying the effects of glucagon are still not clear. In this review, recent research on the mechanisms by which glucagon and its receptor contribute to the pathogenesis of diabetes as well as correlations between GCGR mutation rates in populations and the occurrence of diabetes are summarized. Furthermore, we summarize how recent research clearly establishes glucagon as a potential therapeutic target for diabetes.
Diabetes Care. 2012 Apr 19;35(6):1364-1379. doi: https://doi.org/10.2337/dc12-0413
Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).
Glycemic management in type 2 diabetes mellitus has become increasingly complex and, to some extent, controversial, with a widening array of pharmacological agents now available (1–5), mounting concerns about their potential adverse effects and new uncertainties regarding the benefits of intensive glycemic control on macrovascular complications (6–9). Many clinicians are therefore perplexed as to the optimal strategies for their patients. As a consequence, the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) convened a joint task force to examine the evidence and develop recommendations for antihyperglycemic therapy in nonpregnant adults with type 2 diabetes. Several guideline documents have been developed by members of these two organizations (10) and by other societies and federations (2,11–15). However, an update was deemed necessary because of contemporary information on the benefits/risks of glycemic control, recent evidence concerning efficacy and safety of several new drug classes (16,17), the withdrawal/restriction of others, and increasing calls for a move toward more patient-centered care (18,19)…
